Cardiology Breakthrough: How Kidneys Poison Hearts
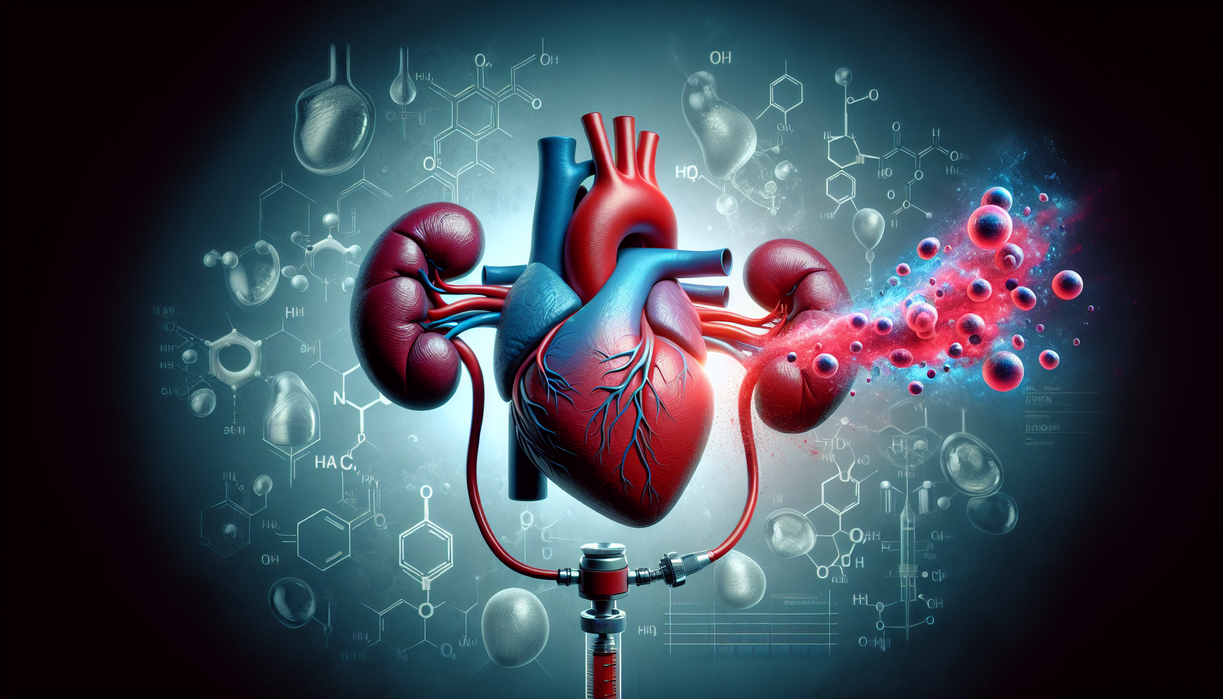
thebugskiller.com – Cardiology has long known that chronic kidney disease shortens lives, yet many patients do not die from kidney failure itself. They die from broken hearts. New research in cardiology now uncovers a disturbing link: injured kidneys release a hidden toxin that quietly sabotages cardiac cells, disrupts pumping power, and accelerates heart failure.
This discovery reshapes how cardiology views kidney disease. Instead of treating each organ as a separate battlefield, specialists must now see a connected warzone. The kidneys are not only victims; they become reluctant accomplices, sending harmful molecules into the bloodstream that poison the heart from within.
When Kidneys Turn Against the Heart
For years, cardiology experts observed a puzzling pattern. Patients with chronic kidney disease had a sharply higher risk of heart attacks, arrhythmias, and sudden cardiac death. Their blood pressure was often controlled, cholesterol lowered, yet their prognosis remained worse than expected. Something else was attacking the heart.
The new research points to a specific toxin released as kidney tissue deteriorates. These damaged kidneys fail to filter waste effectively. Harmful substances accumulate, circulate through the body, and eventually reach the heart. Cardiology labs show that this toxic load interferes with the heart’s energy production, disturbs muscle contraction, and inflames delicate cardiac tissue.
From a cardiology perspective, this finding is revolutionary because it turns kidney disease into a systemic cardiac threat. The heart is not merely overworked by fluid overload or high blood pressure. It is actively poisoned by molecular byproducts that healthy kidneys would normally clear away. This molecular sabotage helps explain why standard heart therapies sometimes fall short for patients with poor kidney function.
Cardiology’s New View of Organ Cross-Talk
The emerging concept in cardiology is organ cross-talk: the idea that one failing system can chemically injure another. The heart and kidneys share an intimate partnership. The heart pumps blood to nourish kidney tissue, while the kidneys regulate blood volume, electrolytes, and hormones that influence pressure and cardiac workload.
Once kidneys become chronically diseased, this partnership collapses. Cardiology teams now recognize a vicious feedback loop. Reduced kidney filtration increases toxic molecules, which damage heart muscle and vessels. As the heart weakens, it pumps less efficiently, further decreasing kidney perfusion. Both organs spiral downward together, making recovery challenging.
From my perspective, this shift in cardiology thinking is overdue. For too long, clinical care has been siloed. Nephrologists handle kidneys. Cardiologists handle hearts. Yet the patient lives in one body. This toxin discovery underscores that single-organ strategies are no longer enough. Truly modern cardiology must include kidney health as a core part of risk assessment and treatment plans.
What This Means for Patients and Future Care
This research opens wide possibilities for cardiology and kidney medicine. If scientists can pin down the exact toxin structure, new drugs may block its production, neutralize it in the bloodstream, or help remaining kidney tissue clear it more efficiently. Cardiology clinics might begin testing earlier for kidney-related toxins, not only traditional markers like creatinine. Patients with mild kidney impairment could receive aggressive cardiovascular protection long before symptoms appear. Lifestyle advice would gain new urgency: every choice that preserves kidney function may directly shield the heart from toxic injury. To me, the most powerful message is human. Cardiology is not just about stents, pacemakers, or dramatic rescues. It is about understanding interconnected systems so deeply that we can prevent damage before it starts. Chronic kidney disease no longer looks like an isolated diagnosis; it is a warning flare for the heart. Recognizing that relationship invites a more holistic, preventive, and compassionate form of care, where preserving one organ becomes an act of protecting the entire person.